Introduction
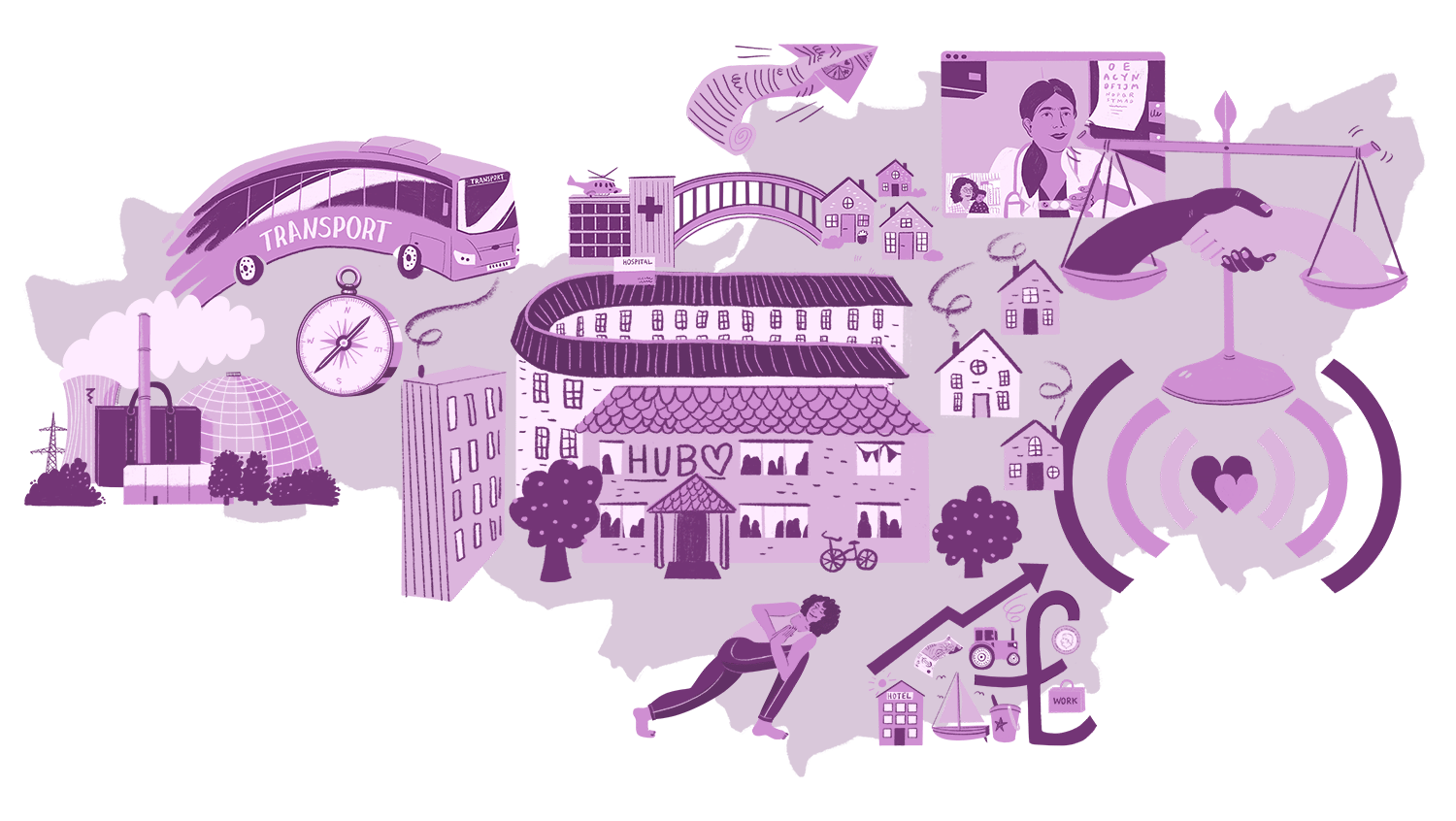
The 'National Wellbeing Service' scenario imagines a future where the systems of Health and Social Care have become integrated into one wellbeing system. It describes a world where personal responsibility for health and care, family and community is accepted by the wider public. There is no stigma for people seeking social or medical care, everyone needs different things at different points of life. Most services are integrated and local through Wellbeing Hubs.
Since the 2020 pandemic, and from a young age, people are taught about their responsibility to look after their minds and bodies. This is a future where people are included in shaping the services that support them in their lives. They feel their voice is heard and they are valued. Many of the growing older population in Somerset and the South West Region enjoy the positive aspects of older age. Acute and emergency medicine are managed as a separate service.
What will it be like in 2035?
The majority of the population in Somerset and the rest of the South West will be taking responsibility for their own mental and physical health.
Public health will drive everything through the South West Wellbeing Service - protection, prevention, public confidence.

Prescription (online) yoga, health coaches, counselling and other personalised therapies will be freely available from the NHS to the Somerset population.
One-stop shop community health hubs will be available across the South West, including Somerset. These partner with health (including GPs), social work, voluntary and private providers to supply high-quality services such as diagnostics, prevention, rehabilitation, and minor care.

There will be a network of residential and nursing care facilities linked to the community hubs, which will also offer step-up and step-down facilities (beds) to enable recovery on discharge from acute services.
Acute and emergency services will be in regional specialised units with relationships to other regional specialisms as needed. A new national acute service will be in place, managed through a national network and a new Government department called 'Heroes', as distinct from the wellbeing service which is led locally through a consortium of Place based stakeholders.
A view from 2035
Today in 2035 a strong community spirit around health and wellbeing has emerged across the South West. Somerset has been at the heart of this since the early 2020s where the 'One Somerset Workforce' strategy and other areas such as Fit For My Future Somerset health and care strategy was developed, aimed to support the health and wellbeing of people by changing the way services were planned for, paid for and provided. Emerging from a decade-long series of radical reforms of services to improve, maintain and restore the health of individuals and communities, Prevention, Protection and Public Confidence have become the watchwords.
Over ten turbulent years the 20th century National Health Service has slowly given way to a 21st century National Wellbeing Service.
From the outset in 2023, Somerset was an aspirational place to be. Chief Medical Officer Dr Bernie Marden in the ICS Primary Care Strategy set the course :
Hope [is] a theme... Patients hope for a warm, caring welcome, attention to their needs and an ability to access care in a timely way. Primary care teams, whether working in GP, dental, pharmacy or optometry services, hope to be able to provide high quality care, with enough time and resources to meet patients' needs and go home with the satisfaction of a job well done. System partners hope that our primary care services can be the foundation upon which our integrated care system can be built, a reliable and resilient foundation to deliver our four shared aims; population health, reduced inequality, greater efficiency, and increased social benefit from NHS activities.
Over many years, Somerset has regularly performed above average, for instance in People Promise indicators compared with the South West Region and with England as a whole.
Somerset has recognised even further the importance of developing an agile and flexible workforce, one in which capabilities rather than outmoded and more limiting role-defined characteristics created capacity for workforce development and delivering positive outcomes.
The relationship between people and service providers swung from the dependency dynamic of the first part of the 2020s which had an over reliance on services operating reactively to illness, to the opposite extreme of independence and self-reliance by the late 2020's.
This swing of the pendulum initially had its own pitfalls in terms of undiagnosed illness and safety. However, by 2035 this dynamic has now settled into a more realistic relationship between people and services, characterised by a model of interdependence in which people, communities, and the state work together to maximise wellbeing in communities.
In 2026, a range of new Wellbeing Hubs were created across the South West Region for clinicians, social care staff, volunteers, and families. These Hubs were created to provide advice on self-care and personal resilience and to help staff to recognise their own 'warning signs' of mental ill-health. Somerset's recognised approach, where the NHS Foundation Trust was recognised as Mental Health Trust of the Year in 2021, has been avant garde in influencing the development of positive approaches to mental health across the region and beyond.
Following the extensive and protracted Covid-19 pandemic Public Inquiry which began in 2022, there is a growing acceptance and appetite from the public to take more responsibility for their own health. A rebalancing of rights and responsibilities led the public to see health and wellbeing as a key lifestyle pursuit. The Inquiry exposed serious flaws with the decision-making processes through which the pandemic was handled at pivotal moments throughout 2020 and 2021, and this resulted in clear areas for change that were accepted and built upon by future governments.

The long-term mental health consequences of the pandemic amongst both the health and care workforce and the general public have been addressed as a policy priority since late 2024. As a result, the spectre of a post-Covid mental health Pandemic has been, to a large extent, mitigated thanks to a change in political, social, economic and technological developments. In Somerset, support from the Mental Health Alliance with Open Mental Health providing 24/7 access to support had been in place since the early 2020s and provided a platform for building caring and supportive approaches.
'Stories of Covid', a campaign by the BBC to highlight the impact of Moral Injury and PTSD in the workforce, led to the 'National Covid-19 Recovery and Restoration Hearings (CRRHs) of 2024. These hearings allowed Health and Social Care staff, individually and collectively, to give voice to the trauma of the UK's Covid pandemic and to distil learning for the future. In the South West, local and regional CRRHs enabled staff holding unresolved feelings and trauma from the experience of 2020/21 to be heard as a way to support recovery as a shared societal activity. A collective sense of restoration was experienced and the narrative of Covid as a period of psychological growth as much as trauma became a shared framing of the Covid years.

As a result of the National CRRH, individually tailored wellbeing programmes were mandated and funded for every NHS and social care organisation. In the South West these were embedded in annual appraisals such that today in 2035 there is an accepted and personalised focus on staff wellbeing across all organisations.

We have been on an impressive journey over the last 13 years. In the early part of the 2020s there were many challenges. Following on from the pandemic, further social and economic unrest emerged. Along with the Russian invasion of Ukraine in 2022, the cost of living crisis emerged, creating inflation at a 40 year high, and resulted in significant industrial action across the public sector, with health and care staff lining pickets across the country for fair pay and acceptable terms and conditions of service.
However, following eventual pay settlements in 2023 and the Russian capitulation to Ukraine in early 2024, a period of relative stability made way for a new approach to be taken following UK Government elections in 2024. As a result of the challenges in the early part of the 2020s, it now provided an opportunity to create a new political narrative which was quickly adopted in the mid 2020s, with political and health leaders beginning to truly grapple with a regional health system that really encompassed the improvement of the social, economic, and environmental conditions in people's lives.
As early as 2024, the South West set in place plans to ensure that every person in the region and every health worker had appropriate and accessible information to protect their own health as well as the health of those for whom they were responsible.
Today, hundreds of organisations, some online and many physical centres can be found around rural (and urban) communities across the South West, including Somerset. They offer a range of health services - and the appetite is huge. The shift in thinking from the NHS as a service-based organisation to community anchor organisations has led to a complete rethink of NHS estate and purpose including the adaptation and selling of large, unfit for purpose buildings to resource new integrated community wellbeing centres. These community hubs maximise the use of technology to increase productivity and keep human resources costs to a minimum. Prescription (online) yoga, health coaches, counselling and other personalised therapies are freely available to anyone who wants them in the South West.
The private sector, through industry bodies, commit to being partners in the Community Hubs, investing business resources in shared wellbeing activities for employees as citizens. The prized, Annual Community Partner (ACP) Award given to industry partners involved in Community Hubs, grew out of a post pandemic collective commitment to rebuild the economy through rebuilding health. The ACP Award was initiated in the South West Region and was taken up as a national award in 2035. The first national award ceremony was held in Taunton, hosted by the Taunton Community Hub where the idea was first piloted.
As an area, Somerset has become a thriving place to be, a transformed area where socio-economic regeneration has resulted in benefits across towns, villages and communities. The opportunities provided by Hinkley Point C, the first nuclear power station to be built in the UK in 20 years, have played an important role in improving social mobility in the South West - making a difference to people who need support.
Today in 2035, Bridgwater has impressively outperformed major regional cities across the UK in terms of productivity and the District of Sedgemoor has seen the largest growth in household income in any area of Devon and Somerset - above the regional average and above cities like Exeter and Plymouth. 1,400 companies have been involved in building Hinkley Point C with 14,000 jobs being supported by the project. £10 million has been invested into four training facilities, benefiting local people and meeting skills shortages in the South-West and across Britain.
In turn, further confidence in Somerset as an area of growth and technological advancement flourished, for instance Tata choosing Somerset as the location for a multi billion pound electric car battery plant that created over 9,000 jobs in Bridgwater. This spectacular set of economic developments has had enormous benefits beyond the financial growth of Somerset - the knock-on effects of prosperity and development have supported traditional artisanal, creative and agricultural work, encouraged healthy tourism in a beautiful area, and given an enormous boost and sense of hope to people across Somerset, a catalyst for healthy physical and mental wellbeing across its communities.

Public confidence is high, and people feel empowered and in control of their own health and wellbeing. Technology plays a massive part in this. Accident and emergency doctors regularly consult specialists out of hours via video link. As well as potentially saving lives, this cuts staffing costs and ends the front door/back door dilemmas that beleaguered pre and post pandemic integrated care strategies. Arguments over responsibility for unscheduled care have become a thing of the past, replaced by a more responsive and collective community prevention approach which reduces illness and interrupts the cycle of crisis management that crippled the health and care system of the early 2020s.
Schools have been a hugely important influence in this seismic shift. As far back as 2021, schools in the South West set about supporting children, young people and their families to deal with the effects of the great pandemic. Leaders took their chance to reform the school experience to support pupils. Today, from primary and secondary school, there is a focus on creating environments that encourage wellbeing, and - along with this emphasis - developing the kind of analytical and empathetic skills, and emotional intelligence, that are impossible to 'automate away'.
Pupil wellbeing - both physical and mental health - is prioritised above all else, and pupils are encouraged to pursue their own interests in creative ways, with less focus on rigid curriculums. A decade on, across the South West, we are reaping the benefits with an innovative young workforce who want to stay in the South West and build a healthy future for themselves and their wider community. The local food production, leisure and tech services industries are three significant areas of economic growth in the South West that have stimulated wellbeing and integration across numerous indicators.
Tackling wider health issues and habits was also a priority. In 2032, Edward Hyde, the newly appointed Mayor, declared the South West as the first region in England to be smoke free, with less than 5 percent of the population in Somerset choosing to smoke tobacco, reduced from the 11% of 2023. The Smokefreelife Somerset service amongst other earlier interventions have continued a narrative where unhealthy habits such as smoking are increasingly unpopular. Of course, there are some in society who refuse to give up unhealthy lifestyles, giving rise to less tolerance and a lack of empathy for those perceived to have brought ill health upon themselves. In 2023, 62% of Somerset residents were classified as overweight or obese; this is now almost half of that figure in 2035, with improved education and affordable healthy foods being key factors for the public.
Self-management is central to reducing the need for health care services, particularly in the traditional acute hospital sector where unit costs are high. Now, user-friendly personal monitors and new technologies allow many patients to manage their conditions at home and facilitate seamless transitions between hospital and home and supported by new self-assessment and trusted assessor (for specialist assessments) approaches.
From as early as February 2023 in Somerset, initiatives such as the 'Ready To Go' Units at Musgrove Park and Yeovil District Hospitals were developed to support patents to use activity to avoid returning to hospital or the need for external care inputs.
"We want people to be as independent as possible," said Jannine Hayman, senior matron for integrated and urgent care at Musgrove Park. Initiatives such as this became catalysts for further wellbeing approaches being integrated across all communities in the South West.
More than 80% of those deemed to need care or support receive it in their homes from a range of professionals, but mostly from new Health and Social Care practitioners (HSPs), who, as part of a multidisciplinary team, keep colleagues in the loop on how patients are doing. Information transfer and communication has become the number 1 priority for Multidisciplinary teams leading, in 2030, to the establishment of a new 'Wards on the road” model to support coordination of care and handover. The reference to 'wards' was acknowledged as a bridging term between the previous hospital-based model of care and the new community-based model of care. In 2035 this language is now subject to review, as confusion between place based 'wards' and the now less familiar hospital 'wards' begins to sidetrack staff who report lack of clarity about the purpose of the communication model. This in itself is seen as an indicator of transition from hospital and service-based mindsets to community and place based mindsets, and those staff representatives who had raised the confusion now see this as a positive change indicator.
Increasing workloads mean that these new peripatetic HSPs often end up working longer hours than they are paid for or have to leave without finishing some of their tasks to the detriment of the person they are supporting. This is mitigated for many staff by the new workforce schemes, established post Covid, that recognise 'effort' alongside 'targets'. These have had a significant motivating influence on staff who, following the collective burnout of the Covid years and the significant challenges around pay and conditions, have reconnected to their own personal purpose as care providers and who feel valued and rewarded by both their employers and the public for the role they play in wellbeing.
Today in 2035, supporting communities to act for themselves, for example through community navigators and driving social prescribing, there is now an emphasis on self-assessment for staff and technology enabled portals in IT systems connecting service users, patients and professionals, and the evidence is emerging that Integrated Teams produce better wellbeing and more resilient staff, who risk share and mitigate risk together.
The need for high speed broadband services across the South West to support virtual communication and hand overs led to investment in IT infrastructure and resources in South West communities and with an upswing in connectedness, quality of life and career opportunities in the Wellbeing sector, recruitment to professional roles is at an all-time high in the South West.
The role of Artificial Intelligence (AI) has developed to provide a number of innovative ways of supporting Somerset's citizens with health and wellbeing. After the concerns of academics, the media and AI professionals were raised in 2023 relating to the dangers of AI, the UK Government, along with others across the world, created effective regulatory measures and protocols to mitigate the misuse of AI, including its use in health and care settings.
A study carried out by researchers at the University of Exeter based on early pilot schemes concluded that while a small number of older people were naturally resistant to mobile care (Mcare), self-management had the potential to save millions of pounds through reduced hospital admissions and other interventions. Each year more progress is made and risks mitigated by community navigators and community champions who have enabled digital use and reduced digital disadvantage.

Over the last decade there has been a seismic shift to proactive, social and preventive models of care rather than reactive and medical models - guided by universal care for all, a new shared purpose for wellbeing is held across all stakeholders in the South West. With growing knowledge of what wellbeing means, communities now enjoy personalised care and support planning is now at the heart of all decision-making in the South West.
As preventative and early intervention approaches gained momentum, staff and financial resources that had traditionally been used to respond to crisis interventions could now be redeployed. Significant advances had been made as a result of investment and research, with some strident developments in the prevention and treatment of cancer and other morbidities.
The old philosophical and mindset tensions which, since the inception of the NHS in 1947, had regularly impacted on ambitions for transformation are now a thing of the past. In Somerset, the Integrated Care System (ICS) from the early part of the 2020s wanted people to live longer, and in better health – helping them to live as independently as possible for as long as they could.
With the population in Somerset growing from 571,600 in 2021 to 612,300 in 2035, and with the number of people aged 75 and over doubling, this created workforce, budget and logistical challenges, yet it was recognised that around 40% of ill health could be prevented, and this became an aspirational target. This shared understanding that wellbeing is more about preventing illness and promoting good health and less about reducing use of services was a key strategic driver. Health coaching, self-management education and access to peer support with the community have been key to driving this shift.
In a speech given to the system leadership conference in 2034 by Nasim Salatian, Head of the South West's Wellbeing Service, said:
Today, when we talk about 'systems' we have a shared understanding that what we mean is 'Systems of people and place' not 'service systems'
Organising resources and strategies around service delivery is now frowned on as an outdated, selfish and cruel approach. Systems of people and place are embedded in all our strategies.
The pioneering work of Bristol City to 'Reimagine Place in the 21st Century' has led to all Health and Social Care activities happening under the umbrella of 'Our Place' and happening in our homes, community settings, businesses and public service centres.
Following, what was termed at the time,' the death of the high street' in 2020/21, new models of cities and towns began to be reimagined across the South West with the mixed use of residential and commercial centres, local well-being centres, areas designed for the safe use of prams and frames prioritised rather than cars in planning. Towns across Somerset from Frome to Minehead, and from Yeovil to Bridgwater have all benefited from a commitment to town centre rethinking, designing with the residents of communities allowing them to shape both the services and the places in which they live.
Simultaneously, transport infrastructure has improved dramatically, and in Somerset there is enhanced provision of public transport services such as regular subsidised bus services linked with direct access to the train network where there are increased, regular and fast services in the region and beyond. The cost of public transport has dramatically reduced due to reinvestment of money previously spent on crisis intervention services across the UK and a realignment of some HS2 funding into 'regions of rurality'. The commitment to environmentally responsible 'green' transport has enabled more people to enjoy a range of cultural and leisure opportunities, as well as access to services in the region and beyond. There are well-placed linkages between the Peninsula and major regional (e.g. Bristol, Cardiff metropole) and national (e.g. M4/M5 corridors) high value, technology and knowledge economies.
Acute health needs are addressed through the newly established Acute Care Centres (ACC's) which has been set up and invested in by a collaboration between UK Government, scientists and Industry to acknowledge the importance and distinctiveness of treating medical conditions differently from social and wellbeing conditions.
In 2035, there is a shared recognition of the 30/70% distinction in medical and social determinants of Health, first researched by Sir Michael Marmot in 2020. Acute Care Centres are in their infancy and in addition to infrastructure transitions to move wellbeing activities and equipment into the community, there is an ongoing change and transition programme to help staff and the public make the mindset shift to a wellbeing model of care rather than the medical model of care which the whole population had internalised from the inception of the NHS.
Hospital estates are no longer totemic symbols of health care and instead our old NHS estates have begun a 20-year programme of redevelopment built on the approach taken to the restoration of heavy industry estates across the United Kingdom and Europe where redundant industrial plants are converted into conservation and leisure areas.
Acute Care Centre work takes place in specialist regional units such as emergency units, cardiology and ICU and the bitterly fought debates about which specialism goes to which area was resolved when South West Ambulance Service proposed a radical initiative for their role in enabling Place and Wellbeing initiatives.
From 2035 transport services are split into two service areas - the transfer of patients to ACCs and the transfer of staff to community wellbeing locations (which may be in people's homes). This builds on the work of paramedics working collaboratively with social care and other teams to ensure rapid enablement at home for people at risk of escalating into an acute admission.
In twelve short years we have witnessed a massive shift in the balance of medical and social paradigms and therefore of resourcing. There is a clearer and more realistic distinction in terms of resourcing and mindset between the medical model that sits beneath acute and emergency medicine and the social model of health that sits beneath the wellbeing model.
The 2028 Act of Parliament (Bill of Health) set out a vision for the new National Wellbeing Service, with a clear distinction between acute and emergency health services and Population wellbeing. In this radical but reality-accepting Bill, the balance of Health resourcing and activity was set at 30/70% medical and social support bringing Michael Marmot's ratio of the causes of ill health formally into line with policy. (Previously, 70% of the cases of ill health were the result of social determinants but 30% of Health Funding was given to social determinants. This changed to 70% funding for social determinants and 30% for purely medical issues).
The role of leadership
In 2035 leaders are recruited, trained and rewarded for collaborative practices and for demonstrable commitment to social change ambitions. Promotion of medical illness service models of care are seen as very outdated. Leaders are expected to manage personal and professional ambitions in line with Wellbeing programme objectives; competition is now reframed as a resource for collaboration and innovation rather than professional or personal rivalry. System leadership has replaced hierarchical leadership as the cultural norm in wellbeing services.
The Somerset Integrated Care System website as far back as 2023 stated:
To meet these challenges, we need to think creatively; working together to find solutions which allow us to improve the quality-of-care people receive while maximising the finances, workforce and other resources we have at our disposal.
It is important we consider how best to support people to live healthier lives, prevent avoidable illnesses and ill health where possible, and when people do get ill, we need to make sure that they are able to get access to the right care and support at the right time. Our focus now will be to consider collectively how we can best make use of what we have to improve lives and prevent ill health.
Leadership is recognised as something that happens at all levels in a hierarchy and across organisations, communities and within families. Senior leaders in any remaining hierarchical organisations now expect to work in multiple leadership domains and can move between hierarchical and collaborative roles easily, in order to accommodate matrix leadership and social system contexts.
The 2021 Health and Social Care white paper set the scene for far reaching legislative changes in governance and commissioning arrangements. There has been a radical shift from the culture of competition established by the 2012 Lansley reforms, and today new legal frameworks shore up a collaborative model of partnership in local systems. Governance arrangements have been reset as system accountabilities with a focus on population health and community resilience.
The new legislative frameworks have placed NHS and local authority organisations into collaborative units in regional as well as local place based systems and, unlike previous reforms, the 2021 changes set in motion reforms which took account of the variability in the English system and legislated for decisions to be made by local system leaders. This has worked well for the South West, as leaders were encouraged to build on historical partnership arrangements to embed a culture of collaboration across the workforce and in partnership with patients and communities.
In Somerset, the Regional Learning Academy was set up in 2024 to provide a formal centre for collaborative leadership, initially focusing on public sector leaders across services and organisations, but growing over the years to include third-sector, community-facing and eventually private sector and business leaders that interface and interconnect, providing positive economic, health, educational, environmental and community outcomes. This ground-breaking approach has opened-up opportunities for similar developments across the country, and uses the “Health of the Whole” approach devised by Massachusetts Institute of Technology's Peter Senge to advocate dynamic, caring and compassionate systems leadership.
Financial incentives in the latter half of the 2020's boosted the development of joint budgets and collaborative commissioning which rapidly became the default approach to commissioning and delivery. This created a shift in expectations about shared ways of working that in turn led to a new normal of collaborative practice and cross system mindsets. Although it took a little time, the more direct “hands on” role proposed for the secretary of state for Health & Social Care in the 2021 white paper enabled the government to build on the experience of Covid to work more collaboratively with local government and NHS partners to connect local and national agendas. Implementation plans and system change ambitions today are the subject of creative inquiry and negotiation rather than imposed, one size fits all models. Today, final decision making about South West issues is left in the hands of local system leaders and is underpinned by a mindset of partnership and shared ownership of outcomes.
Resources for the development of leaders are targeted at this cross-system leadership community. Siloed leadership development activity is no longer funded and clinical leaders in Somerset and the wider South West Region are now routinely trained alongside managerial and civic leaders as a way to develop shared understanding and broader perspectives about the complexities of care needs. Cultures of mutuality are embedded in all OD work with a view to embedding relationships in cross system groups rather than professional groups.
Patient leadership, user led and community leadership are now promoted as a valuable resource for decision making at the level of individual care and also at the level of strategic planning and system decision making.
Opportunities for leadership development for people with lived experience are central to all leadership development and OD strategies and all leadership development programmes include participants with lived experience as members of the cross-system group. The insights and relationships formed in integrated development programmes mean that today, leaders with lived experience are welcomed and valued partners within mainstream system partnership arrangements.
Providers of professional and organisational development are no longer attached to NHS bodies and have shifted beyond the domain of Health orientated think tanks. New community focused arrangements have emerged to support the development of leadership for wellbeing across the community, including the new King Charles III Foundation for Community Wellbeing. The Foundation works with health and care professionals alongside a diverse range of community leaders and sport leaders to promote a model of civic health and wellbeing in which mental, physical, social and economic health are positioned as the 4 pillars of Britain for the future. The King set up the Foundation in 2027, building on his long-standing advocacy of community being at the heart of wellbeing and growth. This has released a wave of patriotism for the Wellbeing Narrative, similar to the post World War II recovery narratives and the South West has bought into this ambition as a driver for change across the region.
Being a patient in the South West in 2035
Josh is 3 and lives in Somerset. Three months ago, after a bout of flu, his Mum suspected that something was amiss. She remembered hearing at the Wellbeing Hub that children who wet the bed, are constantly thirsty, and feel tired a lot of the time could be showing signs of Type 1 Diabetes and should have their blood glucose levels checked. She phoned 111, and after a phone consultation an ambulance car arrived at the house within an hour with a diabetes nurse as the passenger. It was a good spot, the nurse tells Josh's Mum, his blood sugar levels are over 20. It looks like Josh has Type 1 diabetes. They all go off to hospital as paediatric type 1 diabetes assessment is still an acute service.
The Diabetes Group who met at the Wellbeing Hub were great, especially in those early days. They offered the family face-to-face emotional and practical help, along with a nutritionist who helped educate them on how best to balance food and insulin requirements. It was all made much easier with diabetes nurses also located at the Hub and they monitor Josh's HbA1c levels. In three months, Josh has only been at the specialist Diabetes Unit in hospital once, when he was first diagnosed and treated. All of Josh's data is automatically uploaded to the wellbeing hub where his management is remotely monitored.
He's doing well, the family have been on a supported learning journey and have taken responsibility with self-management and have become expert 'carb counters'. Josh's diabetes management is so good, in discussion with the family, he is now being recommended for a free NHS closed loop insulin pump, before he starts nursery, something the family wanted and pushed for. Josh's older sister, his friends, cousins and wider family wanted to be a part of Josh's diabetes journey and took part in many of the families and friends sessions set up by the Wellbeing Hub. This led to many of Josh's immediate circle reviewing their lifestyle and attitude to wellbeing. As a family they joined a community food growing group and the cousins meet weekly on their allotments to grow vegetables for their wider family.
Workforce profile - Somerset
Total workforce size in 2035
The overall size of the Health and Social Care workforce in Somerset has grown by nearly one-third since the early 2020s.
The 'One Somerset Workforce' strategy was in place from the early to mid 2020s aiming to have the right skilled members of staff working together to make the local area a better place to live and work. A commitment to addressing demand and capacity, in particular to address the ageing profile of Somerset's population, encouraged innovative thinking that put the public at the centre. Workforce planning concentrated on creating highly skilled people with skills that were not dependent on existing roles, but on new roles, needs and outcomes.
In 2023, the UK Government published its NHS Workforce Plan. The aims of the plan were to achieve planned productivity improvements, reduce leaver rates and changes to clinical placement hours, address the barriers in length of medical training, increase the number of apprenticeship places and reduce agency spending. Somerset's innovative and ambitious approach has built on this initial plan with strength.
Investing in core staffing and reducing agency staff has been central to strategic planning, and vacancies have been reduced from 11.6% in 2023 to 5% now in 2035. In the earlier part of the 2020s, Somerset invested in a programme approach (known as the Somerset Talent Hub) to create new pathways into health and care roles across the system, improving recruitment and retention, and giving opportunities to a wider range of people particularly from marginalised communities/areas of deprivation.
The 39,000 staff in Somerset are employed by the South West Wellbeing Service, now by some distance the largest employer in the South West. However, the widespread improvements in personal health which have occurred by 2035 have meant that a relatively smaller proportion of staff now work in acute care services, with the fastest growth occurring in social care, new wellbeing-oriented roles and in the independent and voluntary sector.
In 2025, the South West 10-year Regional Economic Development Plan was aligned with a drive for recruitment in the South West Wellbeing Service and wider wellbeing industries. Alongside other key economic innovations such as Hinkley Point-C, Somerset Energy Innovation Centres and Gravity Smart Campus sites, Wellbeing workforce growth is a coherent and progressive key element in Somerset for an area that is committed to economic and socially responsible development through the years leading up to 2035.
As a highly rural county, Somerset has particularly benefited from new initiatives developed in the South West including incentives for new startups, school and college based schemes and talent management pathways based on the Alaskan Nuka model. These incentives were used to subsidise training in wellbeing skills to support career change for adults, and new legislation to promote higher pay and attractive employment conditions for wellbeing staff has led to a thriving recruitment sector and a competitive pool of potential employees.
A positive cycle of recruitment, retention and wellbeing has now replaced the cycle of workforce shortages, reliance on agency staff and safety issues that dominated workforce strategies in previous decades. Where in 2022 £2.44bn was spent on agency staff in England and there were 124,000 vacancies (including 43.6K nursing vacancies), the South West has been a pathfinder region which has successfully explored realignment of spending into wellbeing services and recruited staff in services that are now seen as attractive, both financially and professionally. The plan to reduce the number of agency staff by 45% in 2024 were highly aspirational in Somerset, indicative of the ambition to ensure a stable and reliable permanent staff profile as is now seen in 2035.
Building on the establishment of new Health and Wellbeing Centres in areas such as Devon in the early 2020s, a number of similar centres were opened in Somerset in the mid 2020s, covering areas such as Yeovil, Bridgwater and Frome.
A large proportion of workers with roles in areas including diagnostics, prevention, rehabilitation and minor care now work alongside one another in an integrated and collaborative way, along with other professionals such as therapists and social workers. AHPs in a wide variety of roles are a valuable part of the health and social care system.
These centres - reconceptualised as 'Wellbeing Hubs' during the rebranding of the NHS as the National Wellbeing Service in the late-2020s - represent the main point of contact between the workforce and patients in 2035, with a Hub located in each of Mendip, Sedgemoor, West Somerset and South Somerset areas, and the benefits are clear to see, especially in more rural parts of the county, while acute and emergency staff have become somewhat more concentrated in the county's urban centres, such as Musgrove Park Hospital in Taunton and Yeovil Hospital which were expanded during the mid 2020s.
In 2035 we see a larger proportion of Somerset's Health and Social Care workforce focussed on more preventative, social and proactive methods of encouraging health and wellbeing than in the past, driven by the new shared ambition for improving wellbeing amongst key stakeholders locally and regionally. Wellbeing Hubs in Somerset, for example, have sought to learn from and build upon the Naturally Healthy initiative set up by Devon Local Nature Partnership and Public Health Devon in the early 2010s.
In Somerset, equitable access to nature is a key priority in all of Somerset's urban and rural communities, with the result that the proportion of residents regularly experiencing the richness of Somerset's wildlife, landscapes and habitats has now reached its highest level in decades.
Fastest growing Health and Social Care occupation
80% increase since 2025
The rapid integration of Health and Social Care has led to the vast majority of care workers in Somerset joining the South West Wellbeing Service to be employed as Health and Social Care Practitioners, a role which combines the more traditional responsibilities of a care worker with an increased focus on proactive, wellbeing-oriented care - for example, the provision of prescription health coaching to those who request it. Health and Social Care Practitioners, therefore, make up a highly agile workforce: they are at the heart of turning the far-reaching vision and aspirations of the South West Wellbeing Service into reality, requiring a willingness to adapt to the ever-more diverse wellbeing-related needs of Somerset's population. The rising population of those aged 65 or over in Somerset - which has grown at a slightly faster rate than in the South West as a whole - has meant that demand for workers in this occupation in Somerset has outpaced other parts of the country.
Other key trends
The strength of the post-Covid societal agenda focused on improving wellbeing, and the pivotal role of regional Wellbeing Services in delivering this agenda have helped build the perception of the South West Wellbeing Service as being a highly desirable place to work amongst most of the public. Indeed, successive governments' willingness to back up this agenda with increased levels of investment - reflected in the rising pay levels of Health and Social Care staff - have helped make a career in health and wellbeing a particularly attractive option for young people. Amongst young people, the sense that a career in the Wellbeing Service is both worthwhile and relatively materially rewarding has been reinforced both by the focus on wellbeing in schools and colleges in the post-pandemic years. Along with other transformational areas in Somerset, it is thriving as a social, economic, technological and wellbeing-conscious part of the country which now attracts people to join local cutting-edge workforces. As well as agriculture, food and drink, and tourism, a leading aerospace cluster is centred on Yeovil, and higher-value knowledge businesses are centred in Taunton and the UK Hydrographic Office.
The overall effect of these trends has been an increasingly youthful Health and Social Care workforce, in which any staffing or skills shortages that arise can be reliably filled from the pipeline of passionate and dedicated student wellbeing workers coming out of colleges and universities in the South West and beyond.
Staff survey results
Staff satisfied with their level of pay
up from 38% of NHS staff back in 2019
Staff feeling unwell due to work-related stress in the past 12 months
40% in 2019
Staff feel that their manager takes a positive interest in their health and wellbeing
70% in 2019
Staff that often think about leaving their organisation
28% in 2019
Impact of Brexit on the workforce
The short-term impact of Brexit was to intensify the staffing shortages experienced by services in the post-pandemic period. In 2022 and 2023, a 'Brexit effect' deterring EEA workers from wanting to move to the UK - combined with political pressures relating to immigration policy at national level - severely limited the extent to which services were able to recruit from overseas.
Since then, however, the negative impacts of Brexit in this regard have been increasingly mitigated. Firstly, the growing coalescence around the idea of wellbeing as a core new national priority, especially evident in the education system, began to have a clear impact; much larger numbers of young people actively sought out careers in Health and Social Care, having a noticeable impact on the size of the workforce from the mid-2020s onwards.
Secondly, as the course of Britain's regionalist, investment-led and wellbeing-oriented political trajectory became clear over the mid-to-late 2020s, the Brexit effect which had deterred EEA workers from migrating here even before any new restrictions took effect gradually started to wear off.
A revised approach to managing immigration positively came into force, including the implementation of a wellbeing health visa scheme to encourage high-quality workers to come to work in the UK and enhance the aspirations of the health and care system. After the UK moved to a new, closer long-term footing in its relationship with the rest of Europe by taking up EEA membership on a 'Norway-plus' basis in 2028, numbers of Europeans coming to work in the South West's Health and Social Care services began to increase more rapidly, and have now almost recovered to pre-2016 levels.
The role of clinicians
Clinical teams in 2035 are set up as collaborative, multi-disciplinary teams, with an emphasis on shared accountability and decision making in relation to patient care and service development. Nurse Leaders and Allied Health professionals work alongside medical colleagues in a non-hierarchical team arrangement with decision making held collaboratively and in relation to wellbeing outcomes rather than professional hierarchies. The MDT hosts a range of clinical specialists under the leadership of a Chief Wellbeing Officer who reports directly to the South West Board. In terms of governance, Medical Directors, Nurse Directors and operational Directors including the Chief Executive Officer, all report to the Chief Wellbeing Officer and performance measures are based on wellbeing outcomes and partnership working. Professional interests, reflected in traditional Royal Colleges and Associations, have been replaced with Wellbeing Bodies in which membership is determined by collective interest and wellbeing specialism rather than clinical training.
- Lead Clinicians and Doctors are experts in converting initiatives that have been researched elsewhere and incorporating them into their working practices.
- There is an emphasis on using data to support resource management at a community level, requiring increased resilience to support patients who may have more difficulty accessing services.
- Doctors are experts in rapid decision making. Resource constraints and risk management inform which diagnostic tests are undertaken. The doctor is placed in a greater position of decision making with fewer opportunities to test and sense check.
- Lead Clinicians and Doctors need to consider the impact on wider society as part of the clinical judgement.
- Medical training for doctors now includes mandatory placements in community development settings, Wellbeing Hubs and in private industry to ensure the development of doctors as well-rounded citizens.
- We see a greater emphasis on the volume of data being used to harness more time to care, and supporting the continued development of patient experts.
- The ethical reasoning behind undertaking research plays a major role and is clearly demonstrated to patients. The interest lies in the mental health and well-being of the patient, throughout the research process and beyond. Patients are educated to use the available data to manage their own care where possible.
- With an abundance of data, areas of research and innovation are relatively easy to identify. Innovation is business as usual with technological advances making it easier to adapt.
- Remote learning and simulation-based training features highly.
- There is a greater emphasis on retention in the South West and promoting more flexible working patterns as an incentive to retain staff.
- All professionally qualified clinicians have a responsibility to be 'fit for work', as set out in the Care Act of 2028 and support is available to reduce instances of burnout, such as enforced breaks, reducing the number of clinical hours for more intense roles, increased peer support, support for doctors living, for example, on call accommodation to reduce travel time.
- Doctors are likely to have a greater influence in the education, training and building of the MDT.
- Clinical leadership is now mandatory as part of the clinician's role and forms part of every performance appraisal.
- In addition to clinician roles, a wide range of other health and care roles and AHPs have developed to meet the needs of people, demonstrating a lithe and agile workforce that is designed to meet outcomes first and foremost.
How we got to 2035
Brexit and the United Kingdom leaves the European Union.
The Covid-19 pandemic impacts upon every citizen in Somerset and across the wider UK, with restrictions in England eventually fully lifted in February 2022.
New Integrated Care Services come into being as ICSs are developed, Integrated Care provider networks of GP begin to commission provision and delivery for their community / local place and their specific needs.
Schools and Colleges in the South West start setting about supporting children, young people and their families from the effects of the great pandemic to reform the school experience to support pupils.
Following a period of political and economic disruption, a new Prime Minister is appointed in October 2022.
The Russian invasion of Ukraine contributes to higher geopolitical instability and worsening living standards across Europe, including the emergence of a cost-of-living crisis in the UK.
Significant industrial action across the health system and the wider public sector in response to higher inflation, falling real wages and concerns around staff conditions.
The UK Government publishes its NHS Workforce Plan, setting out independently-verified national-level projections for key job roles over the next 15 years.
UK Covid-19 Inquiry holds first public hearings.
Pay settlements agreed with striking NHS workers.
Russian capitulation to Ukraine paves way for a period of relative economic stability.
BBC 'stories of Covid' campaign to highlight moral injury in the Health and Social Care workforce.
National and Regional Covid-19 Recovery and Restoration Hearings.
General election - the incumbent government loses and opposition parties are invited to form a new Government on a platform to negotiate a new relationship with the EU and introduce a citizens' income.
Regional Learning Academy established in Somerset to provide a formal centre for collaborative leadership.
European Convention on Human Rights re-enshrined in UK law.
South West Digital Wellbeing Hub introduced in the South West.
Community Empowerment legislation is introduced to encourage communities in the South West to take ownership of community assets which are expensive for councils and the NHS to operate, including buildings and public spaces.
Regional devolution referendums are held and passed by popular vote across England, ultimately turning England into a more federal country.
The first Acute Care Centres are established across the South West.
The South West 10 year regional economic development Plan is aligned with a drive for recruitment in the South West Wellbeing Service and wider wellbeing industries.
Creation of waves of new technical jobs with the growing impact of AI.
Regional assemblies created across England, including the South West, with powers devolved to the local level, based strongly on the principle of subsidiarity. Regional elections held. Local activism and community-led citizen participation increases. The South West elects its first regional Mayor.
The NHS rebranded the National Wellbeing Service.
Introduction of a Citizens’ Income and Universal Credit is withdrawn.
Voting age for all elections is lowered to age 16.
Ascension of 2028 Act of Parliament (Bill of health).
The UK joins the European Economic Area (EEA) on a Norway-plus basis after four years of intense UK-EU negotiations.
Care Act set out for Doctors.
General election - a breakthrough number of Independent MPs representing community interests - building on the strength of their local/regional devolution platforms and supported by the newly enfranchised youth - are elected.
Regional assembly elections held.
Newly appointed Mayor declares the South West as the first region in England to be smoke free, with less than 5 percent of the population choosing to smoke tobacco.
General election, a Government is formed.