Introduction
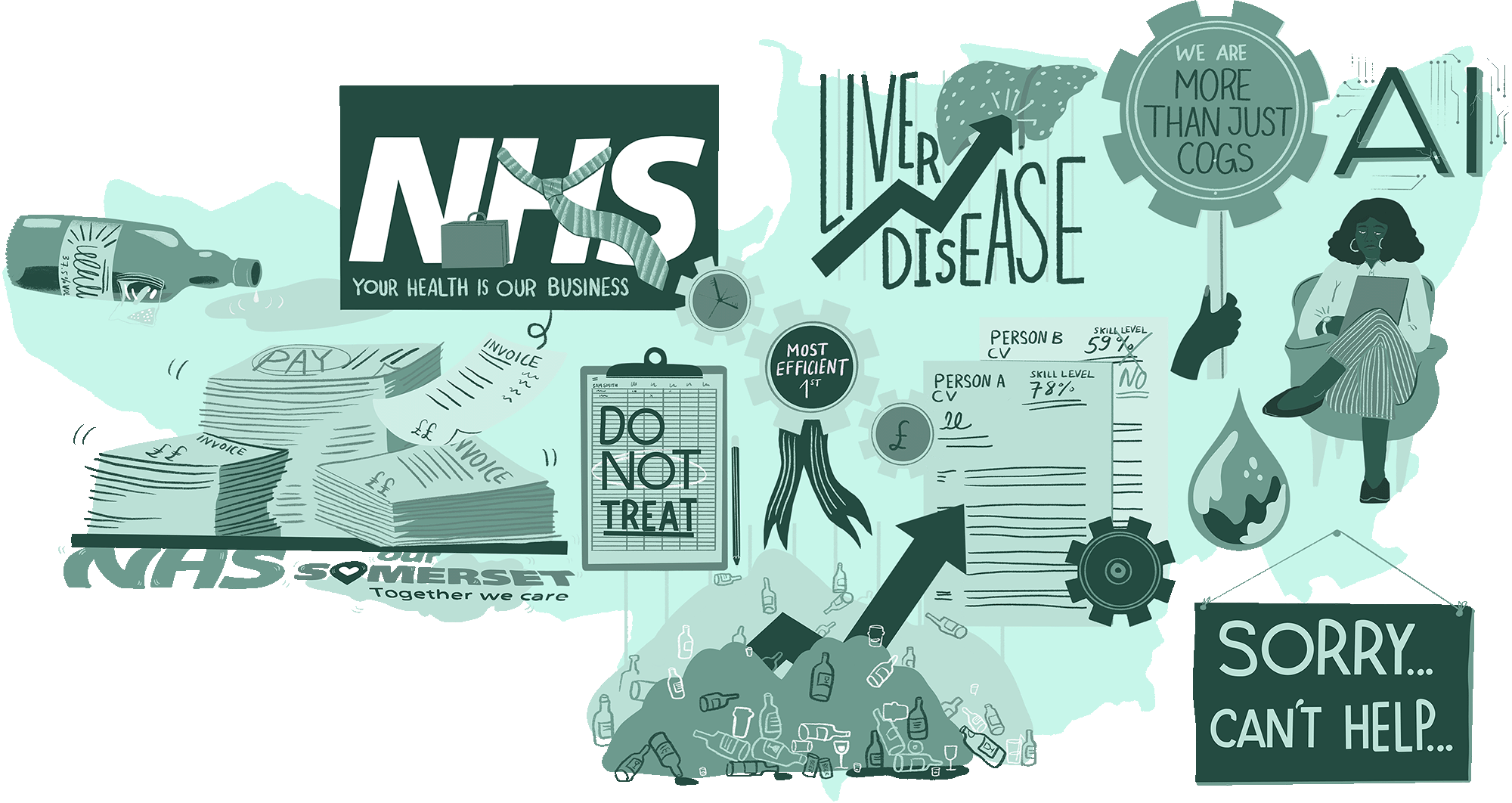
The Treadmill Health and Care System describes a future based on ever-increasing need being put on the NHS and ever-decreasing funding being available. Staff are being expected to do ever-more with ever-less simply to stand still and maintain safe levels of service and care.
The public have allowed this to happen, often through a sense of futility and lack of agency, and politicians have failed to act. Since the Covid pandemic of 2020/21 the public has demanded more investment into the NHS system to try to ensure provision, but the reality is that consecutive reforms have failed to address the underlying issues.
What will it be like in 2035?

Years of increased demand and decreased relative funding will lead to the NHS being unable to offer acceptable standards of care to all.
Integration of Health and Social Care will fail to produce a responsive care system in Somerset and the wider South West Region

Those relying on the NHS will not be able to access many services locally and will be expected to travel or use slow and outdated technologies

The NHS workforce in the South West will be understaffed and many local services will have closed in recent years

Significant demand for staff support will be needed to manage the Mental Health pandemic of Covid and post-Covid unmet demand leading to 90% of NHS resources being spent on traditional staffing.

An emergency health crisis will have emerged, where the combination of significant and widespread poverty, soaring inflation, political instability, environmental catastrophes and significant social discord and turbulence all contribute to a failing system that impacts dramatically on the health of the nation.
A view from 2035
Today in 2035, many commentators report that the NHS workforce feels utterly betrayed. After the tempestuous and often controversial Covid-19 Public Inquiry which hesitantly began in 2022, political promises were made to invest in the NHS which did not materialise. Instead, NHS services began to be dismantled because of funding shortfalls which have impacted significantly on staffing levels.
A failure to address the workforce through a more agile and flexible lens meant that an allegiance to more traditional but restrictive roles could not meet the needs for an ever-changing and more complex world.
In 2023, the Somerset ICS Primary Care Strategy for 2023-2028 stated “we will: 1. Develop a sustainable primary care workforce that can meet the needs of patients and provide a safe working day for our teams 2. Develop integrated teams anchored in their communities 3. Develop a new funding model to invest in population health, continuity of care and access, going beyond the PCN DES. All three actions will be underpinned by a strong primary care provider collaborative, helping our providers to thrive.” In 2035, the irony of this strategic aspiration is not lost, where a demoralised workforce cannot meet the needs of local communities with a funding model that makes little positive impact.
Today, there are few incentives to retain specialist consultants locally with the best being recruited to National Centres of Excellence and Big Pharma. The export of clinical specialists to the US (the UKs primary health partner post Brexit) has left the specialist workforce in the South West depleted, and recruitment and retention are now regular critical agenda items for system leaders, where education and training has dwindled, and the number of places for clinical training across the country has been reduced even further.
There are few specialist centres and large hospitals in the South West anymore and people have to travel great distances, with a chaotic public transport infrastructure, for specialist care.
The hopes expressed in the Somerset ICS Primary Care Strategy in 2023 soon turned to hopelessness. The promises of politicians and health chiefs to work closely with clinicians and other health professionals to identify ways to reduce duplication in how clinical services are delivered translated into deep cuts.
Sweeping changes have been made to criteria for access to services in both physical and mental health services. The initially promising services such as the Mental Health Alliance with Open Mental Health providing 24/7 access to support which had been in place since the early 2020s were simply cut due to lack of funding, ironically cutting all sense of hope for many people in Somerset.
Psychological services are reduced to acute admissions and containment therapies only with a return to 1950s style institutionalised care for large swathes of the South West population.
Talking therapies have become the domain of private therapists and regulation of therapists is now voluntary following the unmanageable increase in individual therapists setting up as sole traders in the aftermath of the cuts to Mental Health services. As a consequence, suicide rates are at an all-time high and the newly established suicide service set up in 2030 to cope with the demand from individuals and families affected by suicide is now overwhelmed. Mental distress is a ticking time bomb for UK society and as a predominantly rural community, the South West Suicide Service has lost track of wider community needs and become focused on Bristol and Plymouth communities only, leaving areas such as Somerset with an abandoned sense of crisis.
Musculoskeletal (MSK) service demand is at an all-time peak and the cut off point for any diagnostic intervention is age 35. GPs are now required to refer over 35s to private sector consortiums of physiotherapists and osteopaths and many larger employers have developed in house deals with private sector providers as a way to mitigate impact on workforce capacity. Beyond large employers, those with private resources pay for their treatment whilst the majority of people with MSK conditions self-medicate with a range of painkillers and steroid treatments available from online pharmacies.
The largely successful economic growth targets for the South West region have been neutralised by the soaring cost of care across all sectors and a financial zero-sum game has been declared by the South West Regional Office for Government.

Successive breakdowns in relationships between system leaders charged with aligning economic and health agendas has contributed to the fragmentation of health and economic factors in the South West. This has shown up significantly in the leadership of local Alcohol Plans. Despite liver disease now being the third largest cause of death in the South West, the development of the 2034 Bristol City Alcohol Plan marked an all-time low in South West integration relationships. On 25 March 2034, the Bristol Economic Wellbeing Board met in Room 1 of Bristol House to approve a £93 million Waterfront Bars and Restaurant proposal whilst at the same time, in Room 2, the Health and Wellbeing Board were signing off a £96 million pound rescue package for a new Liver Unit at Bristol Hospital.
The irony was not lost on community campaigners and a petition was launched by members of the former 2023 Collaborative Communities Forum, demanding that the two Boards meet to align objectives for the Citys Alcohol Plan. The petition did not receive enough signatures to be considered by officials and despite local efforts to mediate between the two Boards, their refusal to meet resulted in two competing strategies for Alcohol in the City being signed off. For political reasons, this was not addressed by the Regional Council in 2034 and today, in 2035 there is confusion and fragmentation at all levels of implementing the Alcohol Plan in Bristol, including different approaches to licensing regulations approved by each Board. Local families and individuals affected by addiction bear the cost of this breakdown of leadership.

The Bristol example is indicative of the breakdown of system leadership relationships across the South West region. In Somerset, the wave of alcohol and other substance abuse has worsened. As far back as 2018, alcohol related mortality in Somerset was estimated at 47.4 per 100,000 residents. This was slightly higher than the national figure of 46.5.
By 2035, this figure had more than tripled to 165.9 per 100,000 residents, and the 5,202 dependent drinkers in Somerset of 2018 had now risen to 17,686 by 2035, well above the average in England. Contributory factors included a combination of economic despair, lack of opportunity in an increasingly isolated rural area and the perception that “self-medication is better than no medication” as one alcohol-dependent resident of Yeovil told the Somerset County Gazettes lead journalist, whose article formed part of a series of sensationalist news stories about the inadequate health service in Somerset.
The long-awaited reform of social care following the increased awareness of the interdependencies between hospitals and nursing homes has led to an increasingly medicalised approach to care of the elderly.
Care homes now fall under the remit of the Director of Nursing and every South West hospital has a Care Dependency Unit (CDU) with limited bed numbers available at any one time for admission. Staff are very stretched in managing this service and there is a constant conflict between NHS and local Government as to who pays for this service to the extent that in 2035 more money has been spent on Judicial Reviews of elderly care in the South West than on the actual provision of care.

Palliative care is reduced to pain management with the 2020s criteria for Do Not Resuscitate stripped back to a Do Not Treat policy which is adhered to in every case admitted to the CDU. Staff burnout in elderly care is high and it is accepted that staff only work in this specialism for a few years. There is therefore little expertise being developed in elderly care interventions and this has become a Cinderella service in terms of R&D.
There is an increasing move towards privatising end of life units as a way to manage demand for care in elderly populations. A confidential paper, drafted after secret discussions between the assisted suicide firm Clementia and the private health insurer BetterHealth facilitated by the UK Government, has been leaked to the press in summer 2035 as a strategy for managing winter pressures in 2036. The paper proposes a strategy for voluntary euthanasia to be available to the over 85s. The BMA ethics committee publicly commented on the leaked paper, saying now was the time to consider all humane options and that the Clementia model of compassion was highly regarded and should be considered as one option to meet the soaring demand in elderly care.
There is an increasing polarisation in the workforce between staff trained before 2020 and newly trained staff. Staff who were trained prior to the acute covid years continue to leave the service disillusioned or suffering from symptoms of moral injury, catalysed by their experience during the pandemic and the persistent retriggering that many experienced in the following years of poorly resourced recovery.
A culture of bullying, harassment and discrimination prevails, with stress, burnout and sickness being the norm in Somerset and across the South West Region.Those who stay are characterised by cynicism, persistent resistance to change and apathy. Many talk about their purpose as one of staying to serve their pension; staff who express a purpose in relation to serving patients are now regarded as naive, dismissed as the moral high horse brigade or the laughable old guard.
A culture of distrust is embedded in the Service, with Trade Unions and Staff Side interventions a daily feature of management activity, leading to chronic delays in decision making, a rise in safety issues and an ever-present fear of litigation which cripple management resources and stifle innovation.
Newly trained staff have gone through a rigorous new curriculum designed around a minimalist health service with career progression rewarded for efforts in efficiencies and meeting targets for reducing patient usage of services. The NHS Graduate Trainee Scheme has replaced general manager training with management consultants training in a groundbreaking transfer of the much loved service scheme to the private sector.
Any opportunity to utilise Artificial Intelligence (AI) in a modern health environment has been poorly managed. Although other countries in Europe, Asia, and North America have made some innovative use of AI, in the UK a combination of lack of meaningful regulation, lack of investment and lack of technological acumen has led to a health service that is at best behind the curve, and at worst fearful of the use of AI. Poor control systems in the mid 2020s when some initial trials were taking place to use AI to potentially mitigate health conditions and manage care in an innovative and efficient way were soon replaced by embarrassing data breaches, unreliable systems and a dearth of strategic thinking.
The public had no confidence, and only basic use is made of AI and wider technology in 2035. The pace of change in world-wide technology was not supported by a pace of change in domestic professional or political leadership at all levels.

The big three management consultants have competed for the past 10 years to deliver the lucrative 5-year training programme. The initial contract, awarded to the consultancy firm Prospectum, led to a root and branch reset of expectations for NHS managers which shifted the culture in South West NHS services to that of a business mindset and financial purpose.
This has been built on by subsequent providers and the NHS Grad scheme is now regarded as a world leading business training scheme. (The new contract for 2035-40 has been delayed in response to the expression of interest in running the scheme from two individual global entrepreneurs who have issued a legal challenge to the procurement process based on a proposal to extend the UK training programme to a global health workforce model).
Values Based Recruitment (VBR), an indicator of innovation, and Good to Great staffing initiatives in the early 2020s have given way to Skill Based Recruitment (SBR), which focuses on technical and financial skill sets and privileges personality traits based on rational thinking, objectivity and emotional detachment.
Congruence, empathy and integrity have been removed from NHS leadership and management frameworks and from NHS Assessment Centre criteria. To be human is to be a machine; to care is to be punished was the title of a suicide letter from an NHS Nurse who took her own life following her 6th clinical leadership application rejection. Her letter, sent to the online BMJ on the day of her death, documented years of systematic disinterest from South West NHS leaders and Regional Bodies. Disinterest in relation to the deterioration of care and humanity in the wards at her local hospital where financial efficiency and discharge were the determining factors in care choices, and where the needs of the patient had become, in her experience, a question that incurred managerial reprimand. There was a short-lived news interest in her story but this was overridden by the BBC breaking news event that leaked the hospitals' inclusion on the list for decommissioning hospitals in 2036 on the grounds of bankruptcy.
Integration has also failed to live up to the promises of a decade ago and the energy for transformation has been lost from the culture of system leadership.
The NHS and local government often find themselves in a struggle against one another when it comes to gaining influence and accessing resources. In 2035 we have a new shared purpose for leadership of integration in the South West public sector - resistance. We no longer pretend that integration is desirable and there is an open collusion, a Faustian pact, between different agencies that protecting siloes is important.
The 10-year Plan for Places commissioned by the new Government in 2024 was written in the South West as a shared act of resistance to the imposition of National Government pronunciations on the nuances of South West identity.
With the national Government preoccupied with post Covid recovery,public Inquiries, continuous industrial action, a burgeoning economic crisis and protests that created damage to social infrastructure, the 10-year plan was approved without much scrutiny and was mostly a rehash of old and contested differences from previous ICS and STP plans. As such it allowed for ten years of legitimised cross system competition and protection of silos in local systems. The revised plan of 2034 is today the subject of a judicial review, with legal action threatened to South West NHS Boards and the new South West Regional Council for failing to ensure integration of addiction services which have been deemed a Government priority for communities in 2035.
There is a Mental Health Pandemic in the general population following the impact of Covid and the failure of successive governments to acknowledge and mitigate this. The effects of physical distancing, social isolation and lockdown during the pandemic increased the mental health challenges for the Somerset population. Mind in Somerset and Citizens Advice both highlighted that loneliness, debt, employment issues and physical health concerns were all contributing to high anxiety, and by the early 2020s there were clear indications that severe mental illness had increased during lockdown, with an increase in self-harm and suicides.
Low level mental health problems including anxiety and depression had increased with Mindline in Somerset taking between 500-700 calls per week in 2020. By 2035, this data was no longer captured due to the year-on-year increases in mental health issues, and the system could no longer meaningfully identify numbers as the majority of people were suffering from a range of mental health conditions.
The Health and Social Care workforce are one group who have been hit particularly hard as the impact of moral injury from the Covid experience and subsequent public Inquiries about the role of government in key factors such as PPE and lockdown decisions reveal that more could have been done to prevent the high UK death toll.

Key research findings in 2022 about the mental health impact of Covid on Health and Social Care workforce were used as political footballs. This acted as an avoidance of confronting the unbearable reality of a Health and Social Care community breaking down instead of a shared national response to the growing mental health crisis. As a consequence, the workforce today is psychologically replete and demoralised.
Addiction is high amongst clinicians and safety events are frequent and under monitored because of the volume of incidents. Occupational Psychology teams are overwhelmed and the 2020 focus on compassionate leadership has been replaced with a focus on dispassionate care as a means of staff survival.
Amongst the general public, demand for Mental Health services is unsustainable and US style street scenes, prevalent a decade ago, are now commonplace with mentally ill and uncared for people sleeping rough, drinking on the streets. This huge volume of unmet need has had a knock-on impact on policing and prison services which are frequently overwhelmed in dealing with not only mental health needs, but a society in turmoil in the widest sense.
Volunteer members of the public take on the mantle of care on the streets and at home, as formal Mental Health services crumble and are only able to deal with acute illness. Admissions to Mental Health wards have increased, and there is a shift in policy to increase beds and reduce community treatments in favour of a community Mental Health policy that is not well enough resourced or trained to cope with the volume and complexity of mild and moderate conditions that now dominate UK health profiles.
Homeless shelters and supported accommodation now only accept female residents in a vulnerability-based criteria that has also seen a 60% reduction in occupancy in 2035 compared to 2025. Winter deaths amongst homeless groups have soared since 2025 and annual temporary morgues to deal with winter mortality across the population have become the norm in 2035 - a familiar and accepted community reality since the Covid third wave of Winter 2021.
In education, following the initial Covid-19 pandemic, it seemed that a sea change would be likely to place wellbeing at the heart of the system. However, with the political and economic instability that the country faced in the early part of the 2020s, academic results were the prime focus for schools. Young people became increasingly pressured by a system that simply cared about results and not people.
School leaders and teachers were also under immense pressure, with Ofsted being granted further powers to 'name and shame' 'failing' schools. The suicide of a Primary School Head Teacher in Yeovil following a negative inspection was largely ignored by the media, where the narrative was more concerned with an 'anti-woke' agenda. Children of all ages were increasingly showing significant mental health issues in a system that cared only about performance.
Wider negative impacts on the population have been felt due to a perfect storm of national and international events. The long and expensive war in Ukraine resulted in Russian occupation of the entire country by 2028, and the world continually sits upon a precipice of nuclear warfare, with rebel-supported Russian troops massed at the borders of Romania and Poland and NATO Alliance nations fearing attack in the early part of the 2030s. This created an international economic spiral with inflation soaring to 30% by 2030 in the UK. Populism has swept across Europe and the US, and far right wing governments are the norm in the UK, France, Germany, Italy and many other nations.
Public sector workers cannot exist on the pay they earn and are unable to pay mortgage interest rates that have risen to 15% due to 'stagflation'. The rental market is accepted as exploitative, and workers such as nurses either enter a pit of debt if they are fortunate to access credit, or are reduced to one basic meal a day.

The industrial action of 2022/23 resulted in minimal pay increases, and the Strikes Bill of 2023 designed to prevent action affecting minimal service provision eventually became the Abolition of Industrial Action Act (2025), making it illegal for all public sector workers to take strike action. Civil unrest is common on the streets of Britain. Looting, robbery and organised violence create fear in communities. The added impact of climate change in Somerset, with unhealthily hot summers, colder winters and natural disasters such as coastal flooding and storms being much more common has put even more pressure on the system. Britain has become a dystopian nation, a land where chaos rules. Nevertheless, those who have benefited from economic and social instability have continued to be rewarded at the expense of the majority.
The World Health Organisation Workforce Support and Safeguard List of Red Countries has been largely ignored, and recruitment of people from developing countries is specifically targeted by the central government to reduce costs. The net immigration figure of 606,000 immigrants in 2023 has now doubled, with the revised Immigration Policy of 2025 the butt of opposition politicians and media scorn. In turn, this has created further social tensions where residents born in the UK feel growing resentment at those arriving, where housing, employment and health pressures are increased. A rise of far right wing organisations are not only to be found in large urban areas of England, but in communities across Somerset where many who identify as white British are angered and propelled by a racist narrative.
Today, commissioning of services is no longer debated as an indicator of need. At best, commissioning of services is a financial exercise to ensure critical services can continue whilst demand is reduced for all other services. At worst it is a managerial and bureaucratic exercise to ensure that accountability for taxpayers money is maintained, prioritising staying in credit financially, with little reference to what is actually needed by patients and communities.
The last South West Integrated Care System Board in June 2035 was held as an emergency meeting following the Boards Summer Report which showed a predicted overspend by £73.4 million in 2035, and the subsequent removal of the CEO and DOF from their roles. The meeting was attended by an NHSE turnaround CEO and interim DOF who gave assurances to the Board that a new regime was being put in place and that providers had been issued with new contracts and budget priorities for service delivery.
Back in 2019, The King's Fund identified a large and growing gap between capacity and demand in district nursing services, with staff reporting feeling 'broken', 'exhausted' and 'on their knees'. There was a 35 per cent reduction in health visitors in England's NHS between 2015 and 2020 and a 38 percent decrease in learning disability nursing numbers between September 2010 and September 2019. These figures doubled between 2021 and 2024 with the result that community services were no longer a viable option, and vocational routes for staff became limited to general nursing roles with limited career specialisms and generic, 'one size fits all' services to patients. Over ten further years, in 2035 demand is sky high and capacity almost non-existent.
The role of leadership
In 2035 leaders are recruited, trained and rewarded for stamina, ability to compromise and flexibility with values. The language of burden, crisis, control and efficiency dominate the South West leadership discourse; despite rhetoric to the contrary, managerialism is promoted above leadership and performance is measured by adherence to protocol, procedure and bureaucracy.
Leaders have consequently adopted an increasingly tight managerial approach, based on centralising work priorities and controlling activity as a way to manage change fatigue and unrest in the workforce. The proposed approach to compassionate leadership advocated by national experts at the Queens Fund (where autonomy, belonging and competence are valued) has been replaced by a new proposal in which rule compliance, working in professional units, rather than across teams and systems, and financial competence are most valued.
The unintended consequence of pressure by the central government means that work needs to be done at a higher level where people in leadership roles are more reluctant to change and politics comes into play.
“We thought the politics issue should sort itself out when we formally integrated as there would only be one organisation and one board. But it didn't, it got worse.”
This comment from a Somerset staff survey revealed the ongoing and now chronic problem with political manoeuvrings and organisational competition locally.
Clinical leadership is discouraged and clinical development is limited to medical specialism as needed. There is an emerging culture which views clinicians as an old elite who have been pampered and over invested in as a profession. In 2035 there is a South West approach to investing in managerial and operational leadership as a way to redress this perceived imbalance and to support achievement of performance objectives.
Turnaround leaders have evolved to become the most powerful leadership roles in the country. In the South West, The Exeter Group as they have become known, are one of the most powerful Networks in the country and are regularly drafted in to sort failing systems across the UK. The Group is used as the benchmark for leadership attributes which include comfort with difficult conversations, assertiveness, single mindedness, the refusal to compromise and the promotion of public humiliation of managers as a performance motivator.
The Group cut its teeth on a seminal turn around process in Somerset in 2029 where two-thirds of the management team in each NHS organisation in the area were removed over a 2-month period. Recruitment giant Hart worked in partnership with NHS Providers and the Turnaround team to source a fully operational, international replacement management team within 6 weeks. Attractive salaries were offered to the new managers for an 18-month contract and when that ended in 2030 staff were let go and services were further centralised under super manager structures of 60 people to one line manager. The savings created by this Turnaround process were significant and a new model of Turnaround was written up by the Group in partnership with Ross Business school who came on board to deliver a ten-year contract for staff development based on this approach.
A new behavioural framework was developed by Ross in 2030, based on the capabilities and behaviours of the Exeter Group. This has been adopted by all NHS organisations as the benchmark for future leaders following a presentation to the Commons Health and Social Care Committee when it convened a special meeting to explore connecting Business agendas and Health agendas at the House of Lords in 2032.
A study exposing bullying, incivility and corporate coercion in the NHS in early 2000's was reframed in 2030 as constructive form of leadership based on assertive, commanding, and collective leadership. The experience of civil contingency measures during the pandemic highlighted the benefits of command and control leadership, such that collaborative and distributed leadership models became redundant in a culture that is now organised around financial efficiencies and management safety. Combined with the financial success of the Exeter Turnaround Group methods, this framing of leadership dominates assumptions and expectations of what is acceptable for leaders in 2035.
Access to personal development and leadership programmes in the South West is encouraged if recommended by your line manager but there is a three-year backlog of applications waiting for approval at the annual assessment meeting.
Being a patient in the South West in 2035
Josh is 3 and lives in Somerset. Three months ago, after a bout of flu, his Mum suspected that something was amiss. Josh often wet the bed, was constantly thirsty, and was tired and irritable for weeks. Josh's mum tried to arrange an appointment with the GP but the first emergency appointment was more than two weeks away. Josh's Mum decided to take Josh straight to A&E. After a six hour wait, Josh was seen and after investigation it was discovered that Josh had suffered from diabetic ketoacidosis (DKA). He remained in hospital for two weeks then was referred to the paediatric diabetes service.
Luckily for Josh and his Mum, the paediatric diabetes services for the South West are located within Somerset so it's relatively easy to get to appointments. Other families from elsewhere in the region have to travel many miles across to access support. A diabetic nurse talks to Josh's Mum and explains that training to manage Type 1 diabetes is largely undertaken through group work but there was none planned for the coming 6-8 weeks; that was dependent on staff being available and if a big enough group of people could be brought together in one place. That was difficult to arrange. In the meantime, a diabetic nurse would try to come out to their house to talk to the family but that might take some time. The best thing for now, the nurse explained, is to look online and wait for us to get to you to go through some training.
Josh's mum feels left on her own to manage and is worried she doesn't have the skills or knowledge to keep Josh well.
Workforce profile - Somerset
Total workforce size in 2035
Overall staffing levels have increased by around a fifth since 2020 across all Health and Social Care services.
However, this represents a relative shrinkage given the much larger increase in the elderly population of Somerset which has doubled since the early part of the 2020s, causing demand for services to rise rapidly both in terms of complexity and in sheer scale. The feedback in 2022 from the NHS Staff Survey in Somerset stated “some colleagues are frustrated with their organisations, have less time for friends and family and more people are coming to work when they feel unwell.” Bullying and harassment, often due to over-pressurised management and hierarchical cultures which promoted command and control' leadership, perpetuated an unhappy workforce over the decade of the '20s. In time, this only worsened and became more ingrained. Somerset continued to face significant difficulties in recruiting new graduates and more experienced specialist staff, with rurality and lack of significant conurbations being significant contributory factors.
The composition of this workforce has also undergone important changes since the early 2020s. The strategic plan of 'One Somerset Workforce' was unable to deliver its desired outcomes. A lack of imagination with workforce planning meant that the more traditional, silo-based approach to skills in pre-defined roles did not allow for any real flexibility with workforce deployment or transformation. This contributed to further disaffection and impacted on staff retention, wellbeing and their ability to meet the needs of the public. The UK Government's 2023 NHS Workforce Plan has failed to translate into any real material improvement.
A general growth in acute illnesses during the post-pandemic years, including a rise in the numbers of people requiring urgent help with mental health crises, has forced resources and attention to be put towards increasing the workforce in 'traditional' acute hospital settings, often at the expense of roles oriented towards prevention and more holistic aspects of health and wellbeing. As a consequence, the proportion of the workforce in nursing and support roles has outpaced projections, while many allied health professions now suffer from severe underinvestment. In addition, many providers in Somerset now struggle to fill vacancies in these roles when they do arise due to a decline in investment in education and training, and increased competition for some kinds of staff regionally and nationally. In the South West, the 8,163 vacancies as of March 2020 had now doubled by 2035, with over 5,000 nursing vacancies across the region.The use of nursing and medicine agency staff has also remained consistently higher throughout the 2020s and early 2030s than in the pre-pandemic era. The £2.44bn cost for agency staff across England in 2022 has now more than doubled to £4.98bn, with areas such as Somerset being severely affected due to lack of local people in the population compared with other parts of England. The aspirations of 2024 to reduce agency staff by 45% proved to be fruitless, with the irony not lost that the opposite has become the case, with 40% more being spent on agency staff by 2035.
Another consequence of declining funding levels (relative to need) has been the creeping closure of many local services across more rural parts of Somerset, with many aspects of specialist care less and less accessible to those outside of urban centres such as Taunton, and others requiring residents to travel outside the county altogether. The Health and Social Care workforce is therefore also increasingly concentrated in those parts of Somerset with the highest density of population and those living in more rural areas suffering even more disproportionately. In addition, the dramatic reduction in the number of AHP roles has significantly impacted on the range of support and intervention required for many of Somerset's residents.
Finally, the mounting health problems experienced in Somerset's population as the 2020s and 2030s have progressed - driven by factors including an ageing population, rising levels of addiction and widespread long-term impacts of coronavirus (Long Covid) on people's physical health - has necessitated a crisis-driven, largely short-termist approach to workforce planning in the county and elsewhere in the South West. The consequences of this include organisational competition rather than cooperation with regards to the recruitment of key staff, stagnating productivity as services struggle with finding the time and resources to trial initiatives with the potential to improve efficiency, and more broadly a worsening of morale among staff in a Health and Social Care system in which different parts often seem at odds with one another. This has in turn led to very high and volatile turnover rates amongst staff in key professions, making long-term thinking and planning even more difficult in this regard.
As a result of poor pay, lack of value placed in health and care staff and often toxic cultures found in workplaces, it is widely regarded as an unattractive and mentally draining environment.
Fastest growing Health and Social Care occupation
34% increase since 2025
Acute, hospital-based services have increasingly been prioritised as they maintain standards within funding realities, with aggressive recruitment drives taking place for extra NHS nurses in response to growing public outrage at growing waiting times for acute care. However, declining investment in preventative treatments and care has had the effect of driving demand for acute services higher still, meaning that there remains considerable reliance on agency and bank staff to complement this increased NHS nursing workforce.
Other key trends
One long-lasting consequence of the Covid-19 pandemic has been a rise in prominence of mental health as a key area of concern for Health and Social Care services: both in terms of the enduring impacts of the lockdowns of 2020-21 on the wellbeing of the population as a whole, and more specifically with regards to the trauma felt by many of the Health and Social Care workers who were at the front-line of the pandemic, which proved difficult for many staff to recover from. In 2021, the population of Somerset was 571,600, an increase of around 41,600 people since 2011. By the census of 2031, the population had increased beyond predicted levels to 613,800, with a doubling in the number of people aged 75 years old and above. West Somerset has the oldest age profile in England. Ironically, young people in Somerset are more likely to migrate to other parts of the country for education and work opportunities that simply do not exist in Somerset. This imbalance of elderly residents now means that in 2035 there are significant and established physical and mental health challenges, placing even greater strain on the system. Furthermore, a shift in deprivation relative to the rest of England has developed, with poor housing quality being common. Around 70,000 Somerset residents now live in a neighbourhood identified as one of the 20% most deprived in England by 2035 (compared to 47,000 in 2021), with the highest levels of deprivation to be found in the county's larger urban areas. Rural communities are also deeply affected by the rise in everyday costs such as travel to work. Many families are now living in working poverty where the household income after housing costs is less than 60% of the national average. Key indicators such as the overweight and obesity rate that was 62% in 2023, and which was regarded as a significant health issue then, is now 78% of Somerset's population, where access to cheap and unhealthy food is the norm.
In response to huge public concern regarding this issue, successive governments have put considerable resources towards helping the NHS deal with Britain's mental health crises, which has mainly been manifested in Somerset by a rapid rise in the numbers of mental health nurses. However, most of these additional mental health nurses find their jobs mostly taken up with addressing the symptoms of the mental health crisis, including rising numbers of people experiencing severe depression; across the Health and Social Care system, overworked staff simply do not have sufficient capacity to undertake the kind of preventative action that may help address the root causes of the crisis.
Staff survey results
Staff satisfied with their level of pay
down from 38% of NHS staff in 2019
Staff feeling unwell due to work-related stress in the past 12 months
40% in 2019
Staff feel that their manager takes a positive interest in their health and wellbeing
70% in 2019
Staff that often think about leaving their organisation
28% in 2019
Staff feeling valued for their work
50% in 2019
Staff that believe they experience autonomy, belonging and purpose in their work
The three pillars of effective leadership established as a benchmark by the DH&SC following a report by Michael West in 2025 and still espoused as the system standard in 2035.
Impact of Brexit on the workforce
The short-term impact of Brexit was to intensify the staffing shortages experienced by services in the immediate post-pandemic period. By the end of 2023, however, the numbers of those leaving the workforce due to fatigue and stress became so large the UK Government instituted new incentives for non-British nationals to come and work for the NHS and in social care.
In particular, a new Immigration Health Payment of £800 was offered to all migrants who took up a position in Health and Social Care within six months of moving to the UK. In 2024, a new variant of Covid-19 had emerged. Initially thought to be a mild variant, China XBC became a more harmful and dangerous form of Covid-19 than first thought, and was especially virulent in a number of countries where the health infrastructure and social distancing policies were particularly weak. This included many Red List countries. As a result of this, normal travel to the UK was at points suspended, and ultimately limited. Nevertheless, for countries identified as hotspots of the new variant, the UK Government began running dedicated flights in 2024 to transport health workers willing to move to the UK. Full two-jab vaccination and paid-for hotel quarantining was provided for all migrating Health and Social Care workers from countries where herd immunity from the new variant of the virus had not yet been achieved.
By the early 2030s, workers from non-EEA countries made up around 15% of the South Wests Health and Social Care workforce - around a doubling in this proportion since 2023. Staff remain so stretched despite this in part because of a long-term, continuing decline in the numbers of EEA migrants willing to come and work in a UK which by now has diverged from the EU quite dramatically with regards to key environmental, social and labour market standards: just 2% of NHS workers in the South West come from EEA countries by 2035 in this scenario, down from 5.5% in 2020. This was further exacerbated by a stringent but deeply flawed Immigration Policy preventing any foreign nationals, including refugees fleeing from danger, from entering the UK unless sanctioned to work in a Health and Social Care setting. All immigrants are deemed as Illegal immigrants and deported to countries such as Rwanda, where a daily flight is now leaving the UK, unless they meet health and care criteria determined by the UK Government.
One beacon of hope in Somerset for economic and social regeneration had been the Hinkley Point-C nuclear power station, which in 2023 promised to create 25,000 employment opportunities, 1,000 apprenticeships and revitalise the nuclear power industry. Now, it was the target of protesters angered by any form of nuclear development. Propelled by the conflict in Ukraine and the impact on energy prices, the battle between anti-nuclear activists who had congregated at Hinkley Point-C and the police had significantly damaged the once positive associations of low carbon electricity generation, and the development was now a symbolic representation of the wide and deep schisms that had emerged in the South West and the country as a whole. Living in a largely rural area such as Somerset means that basic costs like fuel are much higher than in many other parts of the country, and many are living in significant working poverty. As a result, further economic downturn in Somerset was increasingly impacting upon the health of citizens, and a health service with a workforce that was now too stretched and unresponsive to a worsening social situation could not cope with the demands being placed on it. A promising point of economic and social revitalisation was now yet another drain on the much-needed resources of the area, where more traditional areas of work such as agriculture, food and drink, and even tourism are now in significant decline.
Glastonbury Festival, the world's most famous festival, started life in Somerset 1970. Glastonbury Festival created more than 1000 jobs for the wider south west region, accounted for one sixth of annual tourism and during the festival 3,000 people paid for local accommodation generating £500,000 of tourism spend in 2013. Onsite spending at Glastonbury (£32 million) was less than on site spend ( £34) and an overall economic impact of £93m. This annual event boosting both Somerset's reputation and coffers closed its doors on Somerset by 2030 as Somerset was no longer able to cope with the arrival of over 250,000 people each June. The festival continues but has moved to Glouester where the infrastructure is developed sufficiently well enough to host the festival.
The role of clinicians
- Clinicians work hard to manage processes to make certain that particular groups are not excluded, by ensuring that the individual patient is kept at the centre.
- We see the emergence of health consumers, bringing new data and potentially privately purchased test data/results into their interactions with doctors. These make for more challenging interaction with patients when doctors haven't previously seen them.
- There is more emphasis on a shared responsibility/ accountability and diminished, smaller teams making clinical judgements.
- Doctors have self-care deeply built into their training to combat the explosion in mental ill health in the profession.
- Overstretched doctors complain they cannot be expected to know the entire holistic view of an individual patient's complexity. There remains a strong emphasis on supporting patients through shared decision making.
- There has been little or no appetite for considering the role of wider and more diverse health and care professionals and AHPs beyond the more traditional clinician roles that are now set in stone.
How we got to 2035
Brexit and the United Kingdom leaves the European Union.
The Covid-19 pandemic impacts upon every citizen in Somerset and across the wider UK, with restrictions in England eventually fully lifted in February 2022.
Following a period of political and economic disruption, a new Prime Minister is appointed in October 2022.
The Russian invasion of Ukraine contributes to higher geopolitical instability and worsening living standards across Europe, including the emergence of a cost-of-living crisis in the UK.
Significant industrial action across the health system and the wider public sector in response to higher inflation, falling real wages and concerns around staff conditions.
UK Covid-19 Inquiry holds first public hearings.
2023 The UK Government publishes its NHS Workforce Plan, setting out independently-verified national-level projections for key job roles over the next 15 years.
Industrial action concludes with minimal pay increases agreed for public sector workers.
The Government institutes new incentives for non-British nationals to come and work for the NHS and in social care.
General election - the incumbent government loses and opposition parties are invited to form a new Government on a platform to negotiate a new relationship with the EU and explore the introduction of a citizens’ income.
A renewed focus on Place as the boundary for systems is set out as key manifesto priority and as a new 10 year Plan for Places is commissioned by The Government and set as a priority task for every local System.
Emergence of new Covid-29 variant China XBC, leading to the reimposition of restrictions on travel to and from the UK.
The UK Government begins running dedicated flights to transport health workers willing to move to the UK from countries across the rest of the world, with full two-jab vaccination and paid-for hotel quarantining provided for all workers from countries where herd immunity from the new Covid-19 variant has not yet been achieved.
European Convention on Human Rights re-enshrined in UK law.
Passage of the Abolition of Industrial Action Act (2025), making it illegal for all public sector workers to take strike action.
The NHS Graduate Trainee scheme is offered to the market and is awarded to Prospectum who propose a root and branch reset of NHS workforce expectations. A new curriculum based on business skills and demand management is implemented and NHS jobs enter Business School career development portfolios.
More money has been spent on judicial reviews of elderly care in the South West than on the actual provision of care.
Regional devolution referenda are held and passed by popular vote across England, ultimately turning England into a more federal country.
Creation of waves of new technical jobs with the growing impact of AI.
Regional assemblies created across England, including the South West, with powers devolved to the local level, based strongly on the principle of subsidiarity. Regional elections held. Local activism and community-led citizen participation increases. The South West elects its first regional Mayor.
Voting age for all elections is lowered to age 16.
Introduction of a Citizens’ Income and Universal Credit is withdrawn.
The long and expensive war in Ukraine has resulted in Russian occupancy of the entire country, with the situating of Russian-backed troops at the borders of Romania and Poland fuelling fears of nuclear warfare.
Hinkley Point C nuclear power station becomes a target of protesters angered by nuclear development, with battles between police and activists in Somerset symbolising the wide and deep schisms that have emerged in the South West and the country as a whole.
The UK joins the European Economic Area (EEA) on a Norway-plus basis after four years of intense UK-EU negotiations.
General election - a breakthrough number of Independent MPs representing community interests - building on the strength of their local/regional devolution platforms and supported by the newly enfranchised youth - are elected.
Suicide Service established to cope with the demand from individuals and families affected by suicide.
Worsening geopolitical instability contributes to inflation reaching a high of 30%, with far-right populist governments becoming the norm across much of Europe and the US.
Regional assembly elections held.
Scale of increase in low-level mental health problems across Somerset means that data on this is no longer meaningfully captured by local providers, with most people seen as suffering from mental health challenges.
Despite liver disease now being the third largest cause of death in the South West, the development of the 2034 Bristol City Alcohol Plan marks an all-time low in South West integration relationships.
South West NHS Boards and the new South West Regional Council threatened with legal action for failing to ensure integration of addiction services.
General election, a Government is formed.